Greetings to you all! My name is Ryan and I am writing a guest blog post this month. I am currently a 4th year medical student at Georgetown University School of Medicine in Washington, DC who will be starting pediatrics residency this summer – location TBD! In the month of February, I had the privilege of rotating in Lesotho with TTL as well as at the nearby Mokhotlong government hospital as part of an international elective in medical school. Georgetown University has a partnership with TTL, and medical students from our institution have rotated at the site before. I was very grateful for the opportunity to have this experience and learn from both this incredible NGO and the health workers of Lesotho.

My Experience
I lived on the site of TTL, so I got to interact with the incredible staff, enjoy the company of the sweet kids, and witness TTL’s operations first-hand! It was great spending time learning about the services that the organization offers. I had the opportunity to work with TTL on outreach as well as spend time in the safe home with the adorable children. It was inspirational to witness the extraordinary work of the safe home staff, who are all local Basotho, and wonderful for me to have the chance to play with the babies and assist in feedings and diaper changes. That being said, the bulk of my time and experience was working at the Mokhotlong hospital just adjacent to TTL. This is a government hospital that has an wide encatchment area across the Mokhotlong and Thaba-Tseka districts in Lesotho. As such, people will travel hours from community health posts to seeking care for a multitude of conditions. There were five doctors posted at this hospital. We would arrive at the hospital early in the morning for a doctors meeting and hear about any admissions from the call overnight. From there, everyone would break off to his or her respective teams. There was a doctor scheduled for maternity, pediatrics, outpatient clinic, female and male wards, and “casualty” AKA emergency department (ED). As someone who is pursuing my specialty in pediatrics, I chose to spend a lot of my mornings in the pediatrics wards and then go to the ED when finished rounding on the patients. During my time in the pediatrics ward, I was able to advertise the services of TTL to the families of children who would likely benefit from their resources and expertise after discharge. In the ED, I encountered a wide array of conditions including broken bones, lacerations requiring suturing, and infectious diseases like TB and HIV.
My Key Take-Aways
During my experience, I met incredible people and had many profound clinical encounters that will have a lasting impact on my perspective of medicine and healthcare in vulnerable communities. I could elaborate on these stories endlessly; but for the sake of brevity, here are four of my key take-aways from my experience.
1) Work is still needed to combat HIV/AIDS – Despite incredible progress in the last two decades, the international community cannot grow complacent in our fight against the morbidity and spread of HIV/AIDS. Although there are many people living with HIV in the Washington, DC where I trained, it wasn’t until I arrived in Lesotho that I first encountered a patient who died of AIDS and its complications. The global community has made incredible strides to make HIV treatments more accessible through programs like PEPFAR and The Global Fund. Yet with the identification of new global health challenges, the fight against HIV/AIDS has lost some momentum and funding. We need to continue to support cost-effective programs that prevent the spread of HIV and target folks who still are not receiving appropriate HIV treatment.
2) Infant health and nutrition must be a global health priority. In U.S. cities where there are fast-food restaurants on every corner, a lot of my energy in pediatric encounters has been spent combating the culture of excess in the American diet. It thus required a mental shift to counsel in the setting of malnutrition and food insecurity that I encountered in Lesotho. More research is emerging that illustrates how the first several years of life influence long-term cognition, health outcomes, and economic stability. Adequate and appropriate nutrition early in development are key correlates of improved health outcomes. Having encountered children experiencing severe malnourishment in the pediatrics wards and in the TTL safe home, I believe childhood nutrition and food security interventions need to be a top priority in the global health agenda. Addressing nutrition in children as early as possible will have a profound impact on both individual health outcomes as well as the economic growth and development of nations. TTL has taken incredible strides to actively seek out food-insecure families to prevent and treat malnutrition while supporting children who are at risk.

3) Practicing medicine in a low-resource setting requires a unique clinical skills set. Having undergone most of my medical education in a setting with unfettered access to technology and advanced testing, when I started working in the Mokhotlong hospital I suddenly felt as if I knew nothing about medicine. There was no CT scanner, labs were limited, there were no specialists, there was no blood available, and the X-ray machine was running out of film. I asked myself, “How can I offer comprehensive care for my patients and make a diagnosis without those resources?” Learning from the doctors and nurses around me, I quickly refined my clinical skills to fit this new environment. I learned to focus on physical exam findings and taking a thorough history. Working with the team, I additionally focused on becoming culturally competent and learning more about the Basotho in order to improve my understanding of their health challenges and needs. This helped me to better connect with patients and offer appropriate care. Consequently, by the end of my experience, I felt equipped with a new
appreciation of clinical medicine and gained skills to take back to my patients in the USA. I additionally realize we can never take the incredible advances in medicine for granted, and we need to disseminate these technological resources to our colleagues around the world.
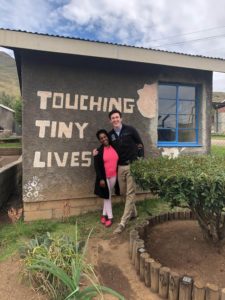
4) “It takes a village.” Yes, I know it is an over-used cliche; but as Lesotho has taught me, it is a cliche because it is so true! Healthcare cannot be viewed solely through the lens of hospitals and doctors. Health starts at the grassroots level, and public health interventions need to be geared to this reality. As such, pediatricians and health care professionals in countries of all income levels need to actively engage in their communities and familiarize themselves with local resources and community stakeholders. That is why I am so grateful to have met and learned from Nthabeleng Lephoto, an incredible, humble change-maker who has given all as managing director of TTL. As a pediatrician-in-training, I’m so grateful for people like her and her team that have dedicated their entire lives to improving the health of kids and supporting families. Pediatricians couldn’t do our jobs without these community health warriors!
Concluding thoughts
Whenever I return to the USA from an experience abroad, there is always an element of “reverse-culture shock” as I reintegrate back into our healthcare structure. Recognizing the privilege of our national health systems, we must not forget how we can support grassroots organizations like TTL and our global community at large. While concurrently, as I reflect on all that I have witnessed and learned, I think that now more than ever that we as Americans should look to Lesotho as of model of profound commitment to community. We cannot underestimate its impact. In the end, there is so much the global community can accomplish when we work bi-directionally!
Lumela, hello! My name is Annie Fort and I am the current fellow for the Touching Tiny Lives Foundation. I graduated with a degree in sociology from Wittenberg University. As a student at Wittenberg, I worked with the Lesotho Nutrition Initiative, a non-profit that packs and ships meals to organizations all over Lesotho, including TTL! Through my experience at Wittenberg and in my current position at TTL, I have learned about Lesotho’s history and the complex issues the nation faces today. I am honored to work with TTL and cannot wait to see what this year brings!


1 Comment
Dr chris mukendi
Mar, 15, 2019It was really pleasure for me to share medicine skills and knowledge with you. Good luck in your future career.